“You get to the point where you’re constantly focused on the next dose,” he says. “You are a slave to it and you realize you’re living in a fog. It all got to be too much.”
The 41-year-old father and active community volunteer had tried to wean himself off prescription opioids before, but the pain would become too intense and he’d soon find himself back on high doses. From his cousin, he learned about Suboxone – a drug used to treat dependence on prescription or illegal opioids – and, after talking about it with his doctor, decided to take time off work over Christmas to give it a try.
“The first few days are a blur,” he says. Having just sold his house following a divorce, he moved in with his mother, who provided emotional support, particularly during the five days he was off work as his body adjusted.
Now, a month later, he takes Suboxone once a day and is seeking alternative ways to manage his pain. These include cutting out foods that cause his arthritis to flare up, eating medicinal marijuana edibles and seeing a therapist.
Suboxone has been available in BC since 2007 and now new regulations that make it easier for health-care professionals to prescribe it. The recent introduction of a less costly generic version has also made the drug more accessible. Suboxone is prescribed for patients who are dependent on prescription or illegal opioids, and it’s covered by BC PharmaCare and First Nations Health Benefits.
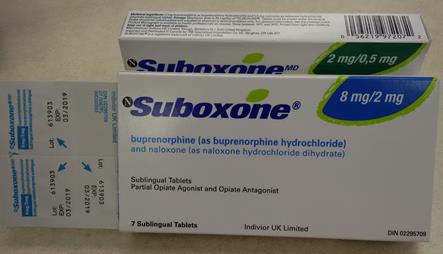 “Suboxone is made up of two different compounds that help treat people with opioid dependencies,” says Dr. Shannon McDonald, Deputy Chief Medical Officer at the First Nations Health Authority (FNHA). “The first, buprenorphine, helps people with withdrawal symptoms, and the second, naloxone, blocks opioid receptors and reduces the likelihood that the drug will be misused.”
“Suboxone is made up of two different compounds that help treat people with opioid dependencies,” says Dr. Shannon McDonald, Deputy Chief Medical Officer at the First Nations Health Authority (FNHA). “The first, buprenorphine, helps people with withdrawal symptoms, and the second, naloxone, blocks opioid receptors and reduces the likelihood that the drug will be misused.”
Because of how the drug works, she says, when someone first starts taking Suboxone, they need to have stopped taking other opioids for 24 hours and be in a state of withdrawal. Patients take Suboxone in front of a health-care professional for the first week or so.
“This is the induction phase,” says Dr. McDonald, “which means getting the patient on a dose that works for them under the close supervision of a doctor, nurse or pharmacist. Once it has replaced the opioid in their system, patients are then put on a maintenance dose that they can take at home.”
“Many people assume that the risks associated with opioid use refers to street drug users when in fact a significant portion of the people at risk are those who have been prescribed opioids for pain relief, often for many years, “says Dr. McDonald.
“Because people build up resistance to the effects of opioids over time, many people have come to regularly use very high doses to achieve the same pain-relieving effects that they felt when they first started using the prescribed medication at a lower dose,“ explains Dr. McDonald.
People often need medical assistance in reducing or stopping these medications – and in finding safer ways to get relief.
Cindy Preston, Health Benefits Pharmacist Lead at FNHA, says that for many people trying to break free from opioids, Suboxone can offer significant benefits compared to methadone, which is also used as an opioid substitution treatment. Methadone is taken in liquid form, often under the direct supervision of a health-care professional.
“There are challenges when methadone is prescribed for clients in non-urban areas,” she says. “On the other hand, once you’re on a maintenance dose of Suboxone, dosing often becomes less frequent, meaning fewer visits to the pharmacy to pick up the prescription. Suboxone is also often better tolerated than methadone, which means that there are fewer unwanted side effects.”
Trish a 31-year-old mother of two who is employed full time – also recently began taking Suboxone. A fall six years ago transformed her life from one of being physically active to one of constant pain. Her doctor prescribed opioids, including OxyContin and methadone, to help her manage her intense discomfort. In September, she finally had surgery to repair her damaged hip, and after the surgery she worked hard to reduce her pain medications.
“I was in a constant state of withdrawal and nausea,” she says. “I was losing so much weight and needed to find other options."
"And I was so done with being sick all the time. I had taken prescription methadone before to manage my pain, but I didn’t like the side effects. Also, since doctors need special authorization to prescribe it, I would have had to go to a different GP. So I decided to try Suboxone.”
Trish says her transition period was difficult, with 12 days of intense illness and three visits to emergency. “I had long-lasting withdrawal symptoms, likely from being on opioids for six years, so my system just crashed.”
After one month on Suboxone, things are looking up. She says she is still in pain, but she’s focused on regaining her muscular strength through water-based exercise.
Mentally, she says, it is a relief “not being stuck to planning your day around your pain meds.” Trish had been taking medication every six hours to try and balance out the highs and lows. But on Suboxone, she takes her dose at night before bed and says “there are no side effects, like terrible night sweats or those hours before your next dose when you feel awful.”
Dwayne’s experience is similar, and he says that the all-consuming need for his next dose that he experienced when he was taking Dilaudid is now gone. He advises other people going through this that while “Suboxone helps with the physical side, it doesn’t necessarily help with where your head’s at.”
The emotional piece of the recovery puzzle is an important one, says Dr. McDonald.
“Social support is really important. Recovery groups and peer support can help as family members and friends may not fully understand what you’re going through. We need to provide love and support for people going through this process – that’s absolutely essential and makes a big difference to those who are trying to change their lives.”
Read part 2 here.

