Coast Salish Territory – The number of First Nations lives lost to the opioid epidemic continued to rise last year even as the overall mortality rates in British Columbia show signs of dropping, making the emergency a severe and persistent threat to our families and communities.
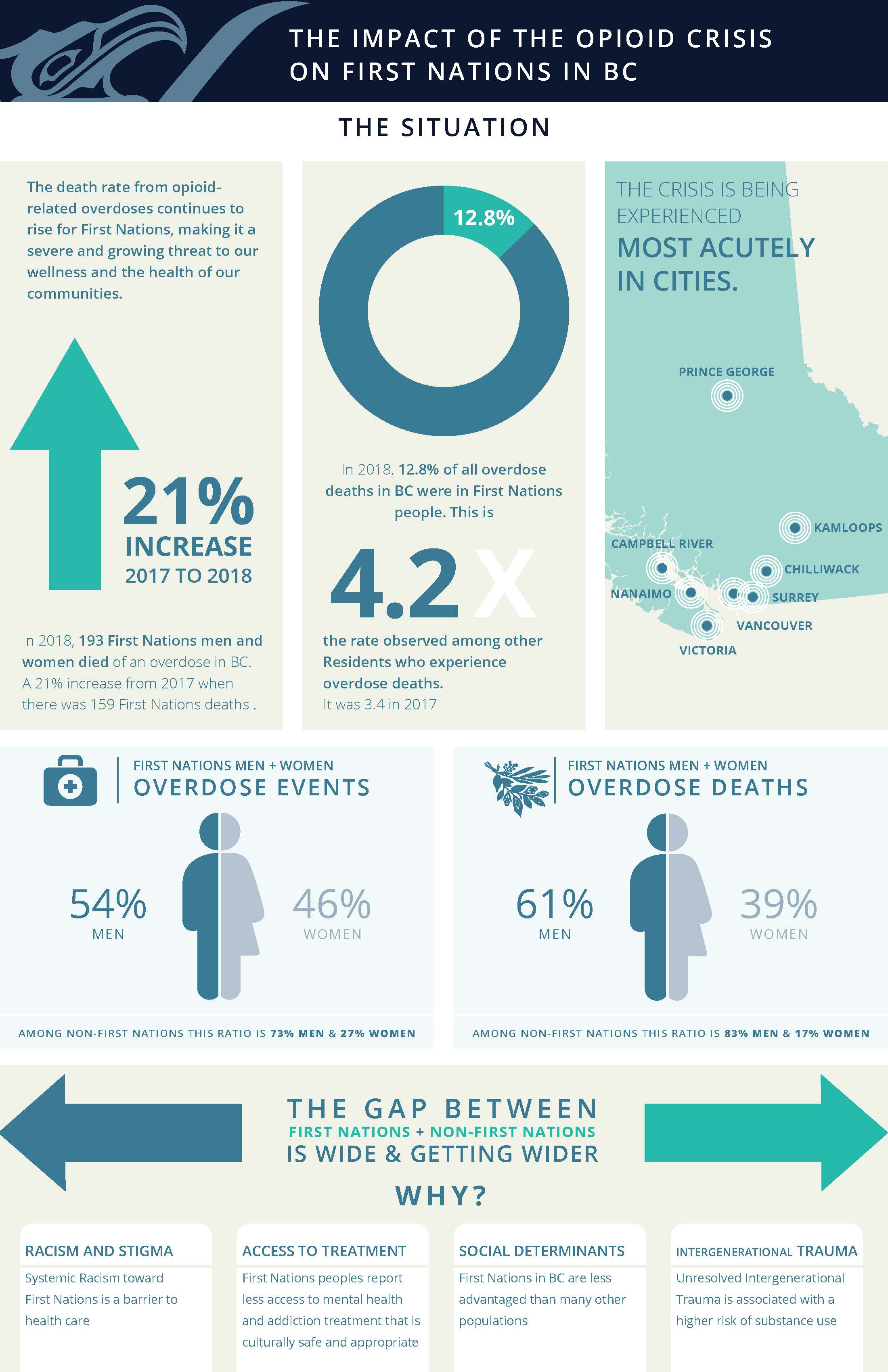
In 2018, 193 First Nations men and women died of an overdose in the province, a 21 percent increase from a year earlier. Overall, First Nations accounted for 13 percent of overdose deaths, up from 11 percent in 2017.
"This is no longer just a short-term emergency, it is a long-term public health crisis that requires a long-term response," said Grand Chief Doug Kelly, Chairperson, First Nations Health Council. "Because of the complex underlying causes that result in First Nations' over representation in this crisis, increased resources and efforts are needed to address the widening gap between the general population and First Nations."
Since the beginning of the state of emergency in 2016, First Nations have been over-represented in the statistics. Last year First Nations were 4.2 times more likely to die of an overdose than the rest of the population. In 2015, this figure was just 3.0.
"There's a strong association between trauma and the propensity for a substance use disorder. Whether that be intergenerational trauma that has impacted families and communities and ultimately individuals, or if it's the ongoing trauma of people's lives" said Dr. Evan Adams, Chief Medical Officer of the First Nations Health Authority. "What alarms me the most is how the gap is widening."
The data reveals how First Nations women are uniquely impacted. In 2018, 39% of all fatal overdoses for First Nations are among women, compared with a rate of 17% for non-First Nations deaths.
"Coroners gather significant valuable information about those dying from drug toxicity in the province and we share this information in support of meaningful prevention efforts," said Chief Coroner Lisa Lapointe. "Our data tells us that, overall, substantially more men than women are dying as a result of illicit drug use; primarily due to fentanyl. Data specific to First Nations people tells a different story. In the First Nations population, women are significantly over-represented, demonstrating a far more significant impact of the overdose crisis on this specific group. Information like this supports important evidence-based prevention efforts."
Community Driven responses to the crisis have been effective in increasing education and services within BC First Nation communities. However, the latest numbers indicate that First Nations living in cities may not be accessing health services to the degree that other people in BC are.
This points to a need for greater cultural safety and humility in health services. There are many barriers to treatment for Indigenous people including underlying systemic racism and experiences of stigma among people who consume alcohol and other substances.
"We have learned that barriers can come down when health care services are culturally-safe and community-led" said Judy Darcy, Minister of Mental Health and Addictions. "Addressing the root causes, and underlying factors of addiction is key to our shared response to this achingly long public health emergency. Together we are making significant new investments to expand on First Nations-led treatment services so they are accessible to First Nations individuals, families and communities across B.C."
Many First Nations people in BC are less advantaged than other populations, creating vulnerabilities related to the social determinants of health like poverty and lack of housing, which are also predictors of substance use disorder and addiction.
"It is distressing to see the continued disproportionate impact of this crisis on First Nations people and particularly women. We know that when women are so affected it means families and whole communities are disrupted. We need to address the underlying causes of the pain and trauma that lead to drug use and addiction." Dr. Bonnie Henry, Provincial Health Officer.
Learn more:
To find out more about First Nations Health Authority, visit: http://www.fnha.ca/
Media contact: | First Nations Health Authority 604-831-4898 |
Backgrounder
Actions taken in 2017/2018
• FNHA provided Harm Reduction grants to 55 communities in 2018 totaling $2.4M. Indigenous Harm Reduction grants provide for Community-Driven, Nation-Based innovative and culturally relevant responses to the Opioid Public Health Emergency, both on- and off-reserve.
• FNHA's Nursing team equipped 8/8 Nursing stations with the capacity to provide suboxone to First Nations community members.
• In just over four months since implementation, 105 clients have experienced increased access to OAT through assistance with clinic fees
• FNHA has hosted Medication Return-It events in 50 First Nations communities, collecting more than 242.5 lbs of discarded medications from 314 households.
• Intensive case management teams exceeded their provincially mandated target by 50%, serving 662 clients in a year.
• FNHA's Unlocking the Gates program has assisted 26 First Nations women and 1 First Nations man transition safely into the community with the required social resources after being released from incarceration
• FNHA increased investment in 6 of 9 FNHA funded Treatment Centres to expand access, and support to individuals on opioid agonist therapy (OAT)
• FNHA has equipped over 2430 community members from more than 175+ First Nations communities with the training and skills to prevent overdose deaths and save lives.
• 3655 naloxone kits were distributed through First Nations distribution sites
FNHA is incorporating the wisdom of First Nations People with lived experience (peers) in its response to the overdose crisis.
• FNHA created 2 First Nations Peer Coordinator positions in Dec 2018 to work at the Crosstown Clinic in the DTES. These coordinators meet and support First Nations people who are using substances at the clinic and in communities around the province and then connect them with First Nations culture through the 'Culture Saves Lives' organization.
• Establishing Regional Peer Positions throughout the Province. A $0.5M annual investment
• As part of the Compassion Inclusion Engagement initiative (CIE), FNHA engaged a total of 273 peers to date to develop innovative and sustainable improvements in harm reduction services across BC through facilitated dialogues that build capacity and foster networks among peers and service providers. Since the beginning of the project, CIE have engaged over 357 people, 201 service providers, and 12 Senior Leaders.
Download this news release in PDF format here (PDF 173 KB)
Download the Impact of the Opioid Crisis on First Nations in BC Infographic here (PDF 817 KB)
