The FNHA's Telehealth Expansion Project team (FNTEP) has had an eventful eight months since the last project update with many successes and ground-breaking events in telehealth expansion with First Nations communities in BC.
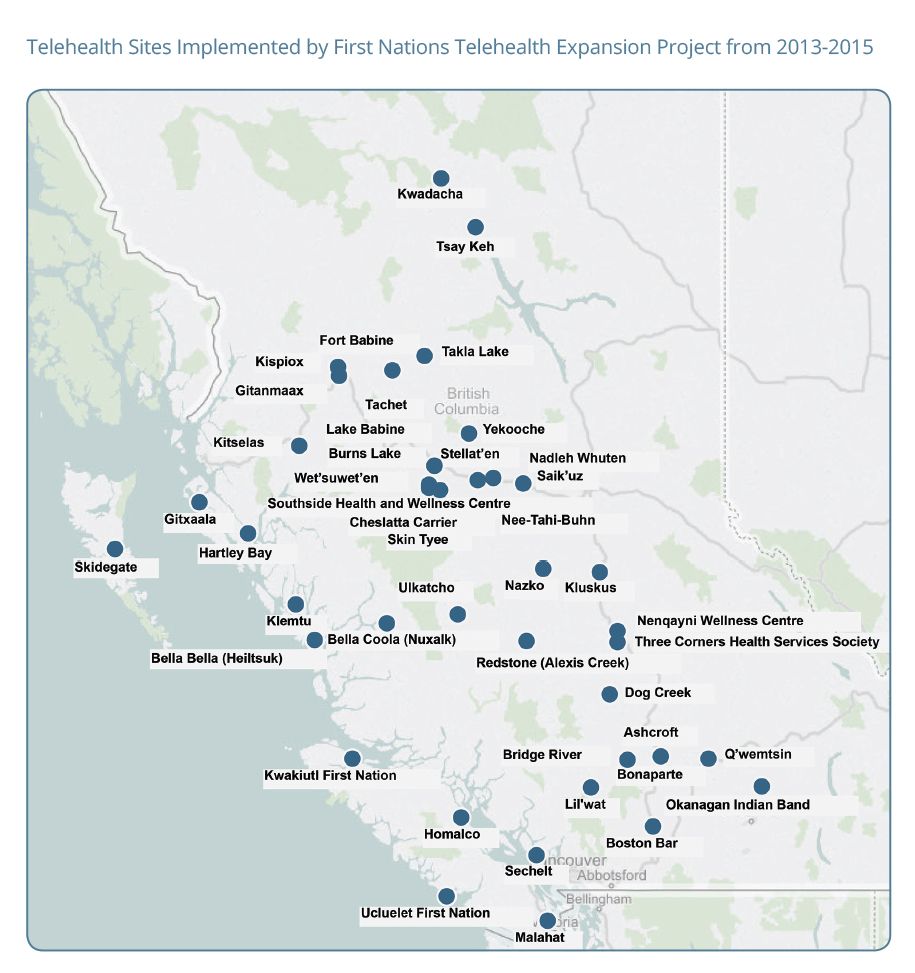
The first wave of expansion since January 2015 has brought telehealth to 18 additional remote First Nations communities in BC (increasing the total number of deployments to 23 since project inception) and engaged 70 new health care service providers – up from just three in January. The service provider network includes doctors, specialists as well as allied health care and family support professionals such as speech therapists, dieticians, physiotherapists, youth counselling and more.
The FNTEP team has also completed 'needs and readiness assessments' with 17 remote First Nations communities in the past eight months. The team works together with community to understand each Nation's unique health care needs and technological readiness as it relates to telehealth.
With success and growing interest in telehealth for First Nations communities in BC, the FNHA is currently working on expanding the Virtual Care Journey of BC First Nations. The FNHA is the process of securing funding for a second wave of expansion in 2016. Over 20 communities have already expressed interest in being a part of Wave 2 of the project. FNTEP hopes to provide specific communication and letters of invitation for participation in January 2016.
The FNTEP team is seeking feedback from community members who have had a telehealth appointment. A short nine-question 'Telehealth Patient Survey' has been created to understand patients' telehealth experiences and collect feedback. This valuable input will inform how the telehealth program develops. Telehealth Patient Surveys can be completed directly after telehealth appointments or are available via email. For any additional questions or comments related to the Telehealth Expansion Project and to obtain a patient survey, please email telehealth@fnha.ca or fax to 604-893-8081.
Telehealth Successfully Delivered to 18 First Nations Communities in BC since Jan 2015
Cheslatta Carrier, Nee-tahi-buhn, Skin Tyee, Boston Bar, Three Corners Health Services Society (Dog Creek, Soda Creek and Main Office locations), Heiltsuk (Bella Bella), Nuxalk (Bella Coola), Bonaparte, Fort Babine, Kwadacha, Tachet, Tsay Keh Dene, Ulkatcho (Anahim Lake), Bonaparte, Q'wemtsin, and Bridge River.
Telehealth Service Provider Network Grows Rapidly
FNTEP ensures First Nations communities have strong partnerships in place with physicians, medical specialists and other allied health care professionals who are telehealth-enabled, creating an ideal scenario for delivering health services to First Nations.
The telehealth team is currently working with 73 health care service providers across BC, up from three service providers at the start of 2015. A huge range of specialties and services are now available to First Nations communities using telehealth including cardiology, dentistry, addictions counselling, pediatrics and more.
FNTEP's Senior Clinical Lead Eyrin Tedesco, works closely with health care service providers and regional health authorities to educate them about the benefits of telehealth, train them in using the technology and build lasting relationships.
The provision of telehealth equipment, software and technical and clinical support by the FNTEP team has contributed the dramatic rise in telehealth-enabled service providers serving BC First Nations. FNTEP's goal is to have 100 service providers confirmed by December 2015.
Range of Telehealth Services Offered Expands Dramatically
Medical Specialties and Services Now Available: Nurse Practitioners, cardiology, endocrinology, Nurse Diabetic Educators and diabetic Nurse Practitioners, Nephrology and Renal Nurse Practitioners, Internal Medicine, Ob-gyn, General and Orthopedic Surgery, Dentistry, audiology, speech language pathology, physiotherapy, pharmacy, child and youth mental health counselling, psychiatry (child and adult), forensic youth counselling, addictions counselling, dermatology, methadone, oncology, chronic disease management, peri-natal and post-natal management, family preservation courses and follow-up, reproductive mental health, pediatrics, rheumatology, dieticians, cancer risk assessment and screening education, respirology, wound care, elder care, infectious disease and HIV/AIDS service providers.
Featured Community Implementations
Boston Bar Clinical Cart Supports Physician Capacity
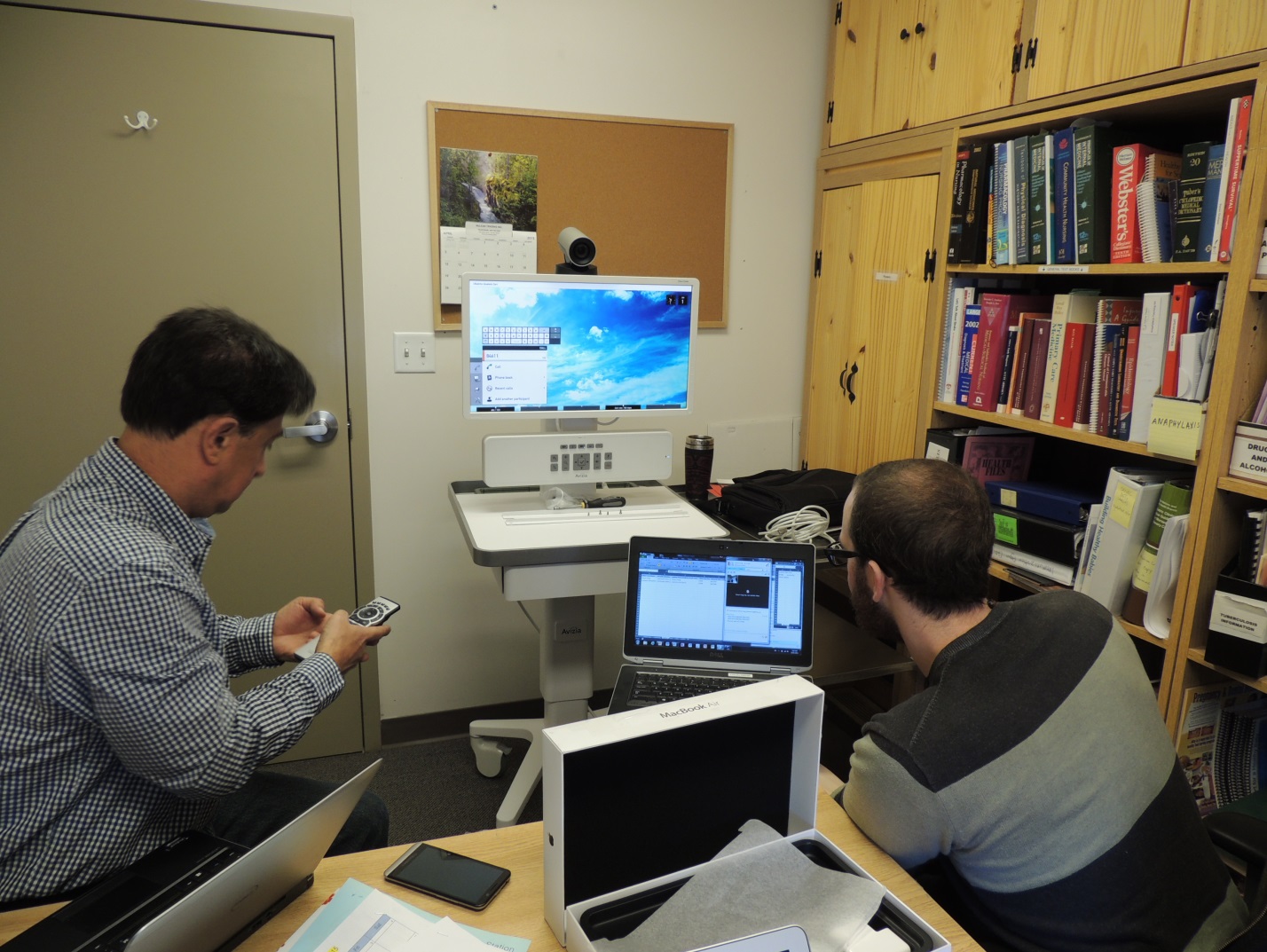
In early August, FNTEP team members travelled to Boston Bar First Nation in the Fraser Canyon to deploy a new telehealth video conferencing unit and clinical cart. The community's physician, Dr. Josh Greggain, is based in Hope and visits the Anderson Creek Health Centre in Boston Bar Nation every Wednesday. Now, with the community's new equipment in place, he can connect with patients between his weekly visits.
"With Telehealth, we now have the capacity to see patients every day. Telehealth gives access to health care when patients actually need the care. Patients don't have to wait for Wednesday anymore," says Dr. Greggain. "On the days that I'm not physically in community I can provide follow-up care via telehealth. I can discuss lab results, CT scans and even provide ongoing chronic disease care – literally anything that does not to require hands-on care."
The telehealth team first visited Boston Bar last year and identified several key network issues that needed to be addressed prior to telehealth implementation. Most notably, upgrades and testing were required in order for the community's network to connect with the Fraser Canyon Medical Clinic, where Dr. Greggain is based. Boston Bar's community health nurse has received telehealth training from the telehealth team and, by simply having the equipment on the premises, ideas are starting to percolate about how else it can be used.
Anderson Creek Health Centre is unique. A local need for health services prompted the community to come together and offer services for everyone in the area, not only to Boston Bar First Nation. The health centre provides primary care, mental health and public health care.
Tachet and Fort Babine have Improved Telehealth Services
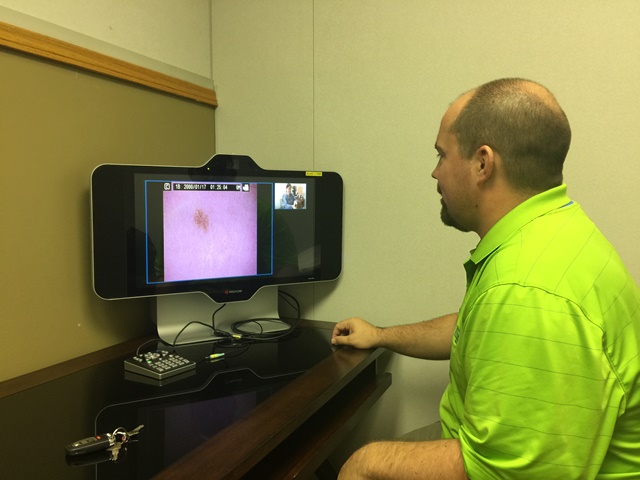
In the first week of June two members of the FNTEP, Telehealth Coordinator Esther Tong and eHealth Support Analyst Stephen Prevost, travelled to Tachet and Fort Babine to deploy and implement new clinical telehealth equipment to each community.
The new clinical carts include clinical peripheral devices which allow physical examinations from a distance. Physicians on the other end can see high-resolution images of the surface of the skin and directly into the ears, nose and throat without patients needing to leave community.
The new clinical telehealth equipment also receives and transmits higher quality video than the old units. The picture and audio quality is very clear with minimal lag time – even though both communities still have satellite connections which usually means lower quality transmission.
The two communities also use their telehealth equipment for non-medical purposes. They use the video conferencing equipment to attend meetings with business colleagues in Lake Babine Nation's office in Woyenne located in Burns Lake, many hours from both communities.
In early April, Esther and Stephen had traveled to both Tachet and Fort Babine to perform a technical assessment to ensure that proper wiring and infrastructure was in place to support the new equipment prior to installation. The team also consulted with local health staff to understand needs, current usage of telehealth and possible improvements.
Three Corners Communities receive Physician and Family Support Services via Telehealth

The Three Corners communities of Dog Creek, Soda Creek and Williams Lake are located in the Cariboo-Chilcotin and before telehealth, the main obstacles to receiving health care services were the lack of availability of physicians in the Williams Lake area and the distance required to travel into town.
Not only is Three Corners now connected to telehealth-enabled physicians, they are also connected to the broad range of family support services provided by the Cariboo-Chilcotin Child Development Centre (CCCDC) in Williams Lake.
CCCDC is keen and fully-committed to providing its full breadth of services to First Nations communities in the region via telehealth. CCCDC has a range of individual and group programs for children, youth and families with a patient demographic that is already 35 percent First Nations.
In operation for forty years, CCCDC has a GP and a pediatrician on staff. Support services include pre-natal support, occupational therapy, speech therapy, physiotherapy, FASD, family support programs and more. The organization prides itself on its cultural-sensitivity and inclusiveness towards First Nations, making it a good match as a service provider for Three Corners.
CCCDC employees are focused on improving access for First Nations. "I'm so excited to be a part of the telehealth project. I want it to be easy for families to get the support they need when they need it," explains Executive Director Nancy Gale. "My biggest hope is to use telehealth to strengthen relationships with community members and staff so that we are getting to the kids that require services as early as possible."
Looking Ahead

Telehealth Training Manual Coming Soon
An FNHA telehealth training manual will support health centre staff in using telehealth equipment for educational purposes, which gives community the ability to attend training and participate in workshops remotely. The manual has been created in partnership with the UBC Learning Circle which is part of the Centre for Excellence in Indigenous Health. The telehealth training manual will be available on-line in the coming weeks.
The FNTEP team works closely with First Nations communities to understand their health service needs and supports the design and implementation of electronic health solutions. The team also provides technical training and ongoing support to the communities they serve, and builds successful partnerships with telehealth-enabled health service providers.
Download this update in PDF format here (932 KB)

