Since the Public Health Emergency was declared in 2016, BC has witnessed an unprecedented number of deaths related to overdoses. The opioid crisis has disproportionately affected First Nations in BC. First Nations populations are five times more likely than non-First Nations to experience an overdose event and three times more likely to die.
Key Milestones
• In April 2016, the BC Public Health Opioid Overdose Emergency was declared, due to the unprecedented increase in overdoses and deaths in the province.
• In June 2016, FNHA developed the Framework for Action: Responding of the Overdose/Opioid Public Health Emergency for First Nations. The Framework for Action describes a set of shared cross-system goals and recommended associated activities for addressing the Overdose/Opioid Public Health Emergency.
• In November 2016, FNHA along with federal, provincial government and organization representatives signed on to a Joint Statement of Action at the Ottawa Opioid Summit.
• On February 17, 2017 BC and Health Canada signed a new 10-year health funding agreement, with a federal commitment to spend $65 million across the country to address the opioid crisis. BC will receive an additional $10 million to help its response to the crisis.
• In July 2017 BC's new government creates a new Ministry of Mental Health and Addiction to improve the access and quality of mental health and addictions services.
• On August 3, 2017 FNHA released a preliminary report: Overdose Data and First Nations in BC
• In September 2017 BC Government budget announcement of $322 million dollars will be dedicated to the opioid crisis
• In September 2017 FNHA applied for and received Treasury Board funding for the next three years, to respond to the overdose/opioid public health emergency.
• In December 2017 FNHA launched a call for proposals for Harm Reduction grant funding.
• In December 2017 the Ministry of Mental Health and Addictions launched a new Provincial Overdose Emergency Response structure. FNHA is fastened into the new structure with both CEO and CMO as members of the Health Sector Oversight Committee, which provides governance.
• In December 2017, the Province of B.C. provided $20m in funding over three years to support First Nations communities and Indigenous People to address the ongoing impacts of the Opioid Public Health Emergency.
• By December 2017, FNHA Indigenous Wellness team reached 126 First Nations communities with Indigenous Harm Reduction training, which includes Take Home Naloxone training
• By December 2017, 1846 naloxone kits were distributed through First Nations distribution sites
• In February 2018, at FNHA's inaugural Mental Health and Wellness Summit, FNHA announced a $2.4m investment in 55 Indigenous harm reduction projects to support Community-Driven, Nation-Based, innovative and culturally relevant responses to the Opioid Public Health Emergency, both on- and off-reserve.
• In April 2018 FNHA added intranasal naloxone spray as a drug benefit. Intranasal naloxone spray is an additional tool to assist immediately to respond and prevent overdose events and overdose deaths.
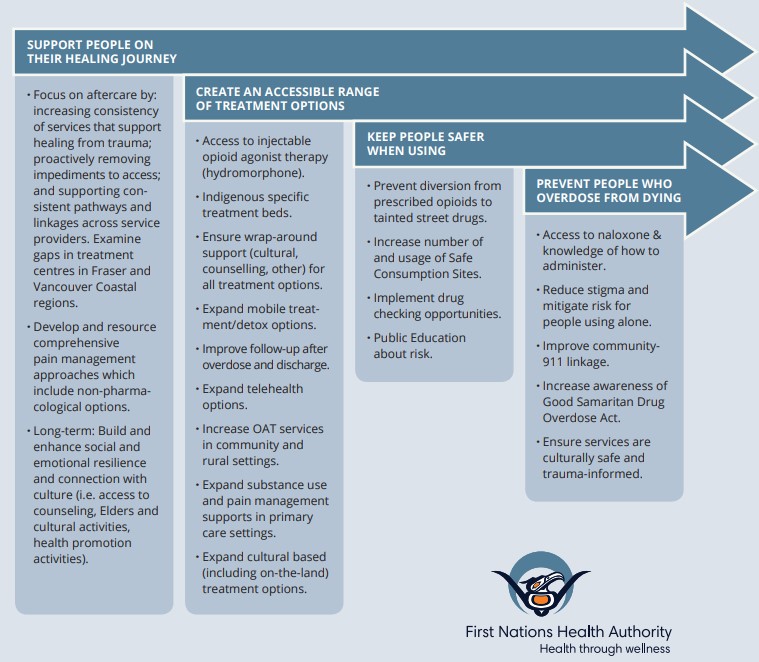
A Shared Framework for Action is developed
In response to the declaration of the public health emergency, FHNA developed a shared framework for action, a framework which BC health partners would work collaboratively within to achieve four primary goals:
1. Prevent people who overdose from dying
2. Keep people safe when using
3. Create an accessible range of treatment options
4. Support people on their healing journey
$20M in Treasury Board Funding over three years
In the fall of 2017, FNHA applied for and received Treasury Board funding for the next three years, to respond to the overdose/opioid public health emergency. FNHA's focuses on the full range of supports and social factors needed to address the overdose/opioid crisis. The initiatives that FNHA will implement are consistent with the Shared Framework for Action including the goal of supporting all health service partners to consider the needs of Indigenous populations. The overall envelope from Treasury Board funding allocated to FNHA is $4 million, $8 million, and $8 million.
FNHA's Opioid Response Plan has Nine Initiatives
FNHA's overdose/opioid plan has nine initiatives that are in alignment with both the Shared Framework for Action goals and the Provincial Action Areas. FNHA's nine initiatives are:
- Expanding Take Home Naloxone Training
- Peer (people who use drugs) Engagement, Coordination and Navigation
- Increasing access to Opioid Agonist Therapy (OAT) in rural and remote contexts
- Integrated First Nations Addictions Care Coordinator roles
- Intensive Case Management
- Clinical Pharmacy Services through Telehealth
- Unlocking the Gates, a Peer Corrections Health Mentoring Program
- Indigenous Harm Reduction Grants
- Communications, Social Marketing, Data and Surveillance
Additionally, FNHA has been and will continue to undertake a review of FNHA programs and operational capacities to deploy resources in support of overdose/opioid response, including FNHA's Health Benefits program, which can enable enhanced access to treatment, and our broader mental health and wellness agenda and programs.
Two new Harm Reduction Workshops
(1.) Not Just Naloxone Training Workshops – The FNHA Indigenous Wellness Team (IWT) is now hosting a new workshop called 'Not Just Naloxone: Talking about Substance Use in Indigenous Communities' (NJN). This workshop supports community champions by building a greater understanding of addiction, substance use, and harm reduction at the community level. This three-day 'train-the-trainer' workshop supports participants in developing community-based strategies to discuss these topics through the lens of cultural safety and trauma-informed care. By the end of June 2018, IWT will have hosted six NJN training sessions: one per region and one urban partner. Read this article for more details http://www.fnha.ca/about/news-and-events/news/not-just-naloxone-training-a-three-day-train-the-trainer-workshop.
(2.) Community to Community Workshops - This is new workshop hosted by the IWT which brings together neighbouring First Nations communities to talk about harm reduction, the opioid emergency, substance use and safety in responding to the crisis.
Peer Coordination
Peer coordination planning is underway in each of the five health regions in order to bring the voices of people who use substances into service delivery. Currently, FNHA is focused on learning about how Peer Coordination is working with our system partners and engaging in partnerships with service providers to support peer engagement across the province, in the planning, development, implementation and evaluation of harm reduction services across BC. The focus is on cultivating open dialogue, reflective practice and inclusive service planning and improvement through collaborative planning opportunities, and support for intersectional networks across health authorities, agencies and community sectors.
Increase supports for Opioid Agonist Therapy (OAT) - Treatment Centres & Community
Three of the ten FNHA funded Treatment Centres are currently supporting clients on OAT. The number of clients being supported is projected to increase as staff are being trained and empowered to demonstrate competence and confidence with supporting clients on OAT
The FNHA Nursing team has been working with the regions to implement a Suboxone treatment induction training for Nursing Stations, to increase Nursing capacity and confidence to initiate, support and maintain clients on suboxone.
Nursing Services Department implemented the following 5 action items:
1. Hired a Practice Consultant for Substance Use
2. Developed a Nursing Clinical Practice Guideline for Suboxone
3. Enhanced nursing competencies in OAT in partnership with the BCCSU Suboxone education and certification program
4. Updated nursing station formulary to include Suboxone and Clonidine
5. Adding Urine Drug Screen Kits to station supplies
For more details, see this article: http://www.fnha.ca/wellness/sharing-our-stories/fnha-nurses-help-build-capacity-in-three-remote-first-nations-communities
Indigenous Harm Reduction Grants
In December 2017, FNHA launched a call for proposals for Harm Reduction grant funding for Community-Driven, Nation-Based innovative and culturally relevant responses to address the overdose/opioid public health emergency. FNHA allocated $2.4 million to fund 55 harm reduction projects to support a range of non-judgmental approaches and strategies to enhance the knowledge, skills, resources, and supports for individuals, their families and communities to make informed decisions to be safer and healthier. To view a map of projects please visit https://www.google.com/maps/d/u/0/edit?mid=19vxG7nMighlOpspWJuLAXXVYEpxFPlWp&ll=53.03683812703193%2C-125.64343414999996&z=5
Intensive Case Management (ICM)
FNHA Intensive Case Management initiative will connect with their respective regional health authority to focus on First Nations clients who have complex needs and are at-risk of overdose to provide culturally safe system navigation and case management supports.
FNHA Regional Teams are leading the implementation of the Intensive Case Management initiative as part of FNHA's overall opioid/overdose response. FNHA's Regional Teams are connecting with their respective regional health authority to focus on First Nations clients who have complex needs and are at-risk of overdose to provide culturally safe system navigation and case management supports. Intensive case management acknowledges that many services and supports are needed to enable an individual that is experiencing problematic substance use to be more successful. Services and supports may include stable housing, adequate financial support, harm reduction, and access to medical care.
Unlocking the Gates
As the evidence shows, the first few days following discharge from prison is a time of high risk for overdose. UBC and FNHA Peer Health Monitoring program provides support and outreach programming aims to assist transitioning men and women in accessing the health and social services they need to increase their chances of a successful reintegration, by improving discharge case management. Program participants receive support that might include meeting a peer at the prison gate, accompanying them to the social assistance office or assisting them in acquiring safe housing, clothing or a family doctor.
The Integrated First Nations Addictions Care Coordinator Role
This shared position with the BC Centre on Substance Use and FNHA will examine the potential innovations to address the opioid crisis by linking into BC Centre on Substance Use's network of researchers, work within FNHA, and with partner organizations to implement strategic, preventative, and treatment-related innovations. This shared position will also dedicate time to improving coordination among FNHA and partner organizations to implement innovative responses, identify and address gaps in service, and ultimately to reduce overdose events and overdose deaths amongst First Nations.
Healthy Medication Use in First Nations communities
FNHA is providing funding to support all First Nations communities in BC that want to organize a Medication Return-it event in their community. Community partners join forces for 'Med Return-it' events and collect unused or expired prescription (or non-prescription) drugs from communities. As of June 29, 2018 three med return-it events have been held and 27 grant applications have been received.
Public Education
FNHA has developed an information portal at www.fnha.ca/harmreducation and a series of Resources for Overdose Prevention and Harm Reduction. The most popular resources include:
• Shane Baker Poster Series Poster series profiling Shane Baker's story of recovery.
• Talking About Substance Use The Do's and Don'ts of having conversations with loved ones who are using substances. Beginning that conversation is a crucial first step. When we are supporting people who are using substances, it is important to focus on building relationships based on safety and trust. There is no perfect formula for having these conversations. This list of Do's and Don'ts will help family and friends get started.
• 5 Myths About Addiction This resource educates friends and family by debunking the top five most common misconceptions about addiction. Learning the 5 Myths provides people with the knowledge they need to reconsider their attitudes towards people struggling with addiction and to consider adopting a harm reduction mindset.
• Overdose Prevention FAQ's The FAQ provides people with all the basic information they need to increase their awareness and understanding of overdose prevention, naloxone, the S.A.V.E. M.E. steps and introduces the new Good Samaritan Drug Overdose Act.
Healthy Attitudes and Beliefs (HABR) Survey
FNHA is currently surveying First Nations and Aboriginal people in BC to learn more about our population's perspectives on the opioid crisis and harm reduction approaches. The results of conducting this survey among 2,000 First Nations and Aboriginal respondents will improve how FNHA delivers health programs, services, and shares public health information with BC First Nations.
Partnerships
The Ministry of Mental Health and Addiction (MMHA) launched the Provincial Overdose Emergency Response in December 2017, to combat the continuing overdose/opioid public health emergency. The new response re-organized key stakeholders to form a Provincial Operational Coordination Structure. FNHA has representation throughout the structure.
FNHA's CEO and CMO are members of the Health Sector Oversight Committee, which provides governance to the overall provincial overdose/opioid response, including by addressing any budget challenges and approving exceptional service changes within the regional health authorities.
FNHA is a member of the Overdose Emergency Response Centre, which will closely monitor provincial overdose data in real time and coordinate with regional response and community action teams to implement measures on the ground as soon as there is an identified need. Membership will ensure that First Nations needs are embedded in the complete system.
News
Nasal Naloxone
On April 4, 2018 FNHA added Naloxone nasal spray as a benefit. FNHA encourages those at risk of an opioid overdose, and people close to them, to have a Naloxone kit—whether it is injectable or nasal—and the training to use it.
Community Action Teams
The 20 Community Action Teams (CATs) are led by each regional health authority– each team is made up of first responders, local and First Nations governments, front-line community agencies, peer groups, businesses, and government agencies – to provide focused, action-oriented strategies tailed to local needs such as resources and supports like Naloxone, overdose prevention services, drug-checking and social supports.
FNHA is working with each Health Authority Regional Response Teams as well as the Community Action Teams, to reinforce our grounding in the system.

