Media Release
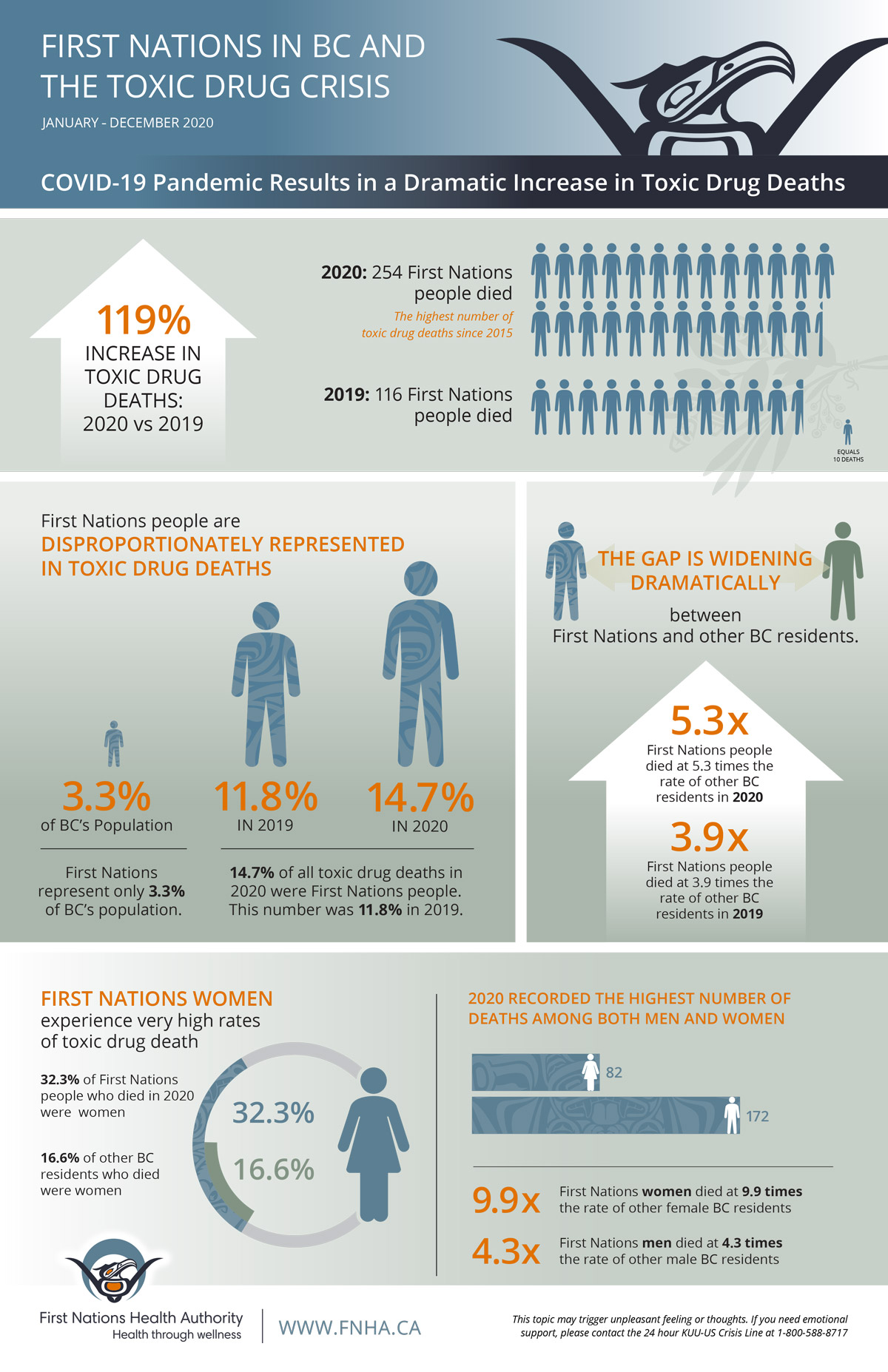
Coast Salish Territory – The number of First Nations lives lost to toxic drugs jumped dramatically in 2020. The large gap in death rates between First Nations individuals and other British Columbia (BC) residents is now wider than it has ever been.
In 2020, 254 First Nations people died due to toxic drugs, a 119 per cent increase from 2019 and the highest number of toxic drug deaths recorded for First Nations since 2016 when the province of BC first declared a public health emergency. First Nations people died at 5.3 times the rate of other BC residents in 2020, up from 3.9 times in 2019.
“The devastating impact of the toxic drug crisis on BC's First Nations people, families, and communities cannot be ignored", said Richard Jock, CEO of the First Nations Health Authority (FNHA). “This issue will not be resolved without the continued support and commitment of health service partners, and First Nations leaders. We must continue to work together to reduce the impact of drug toxicity on First Nations people."
Last year saw the highest-ever number of toxic drug deaths among both First Nations women and men: 172 men and 82 women died. First Nations women were especially affected. Women account for 32 per cent of toxic drug deaths for First Nations people, double the rate of non-First Nations women in BC.
First Nations people have been over-represented since the beginning of the public health emergency. First Nations individuals make up 3.3 per cent of BC's population yet account for almost 15 per cent of toxic drug deaths in 2020. This is an increase from 11.8 per cent in 2019.
The toxic drug supply crisis and the COVID-19 pandemic have had unintended consequences for First Nations people. The implementation of public health measures to reduce exposure to COVID-19 means that more people are choosing to use drugs alone, instead of using with others or accessing harm reduction sites and services. This comes at a time when street drugs are becoming increasingly more toxic.
“The messaging for the pandemic is that we're all in this together but this is not the case for the toxic drug crisis," said Dr. Nel Wieman, the FNHA's Acting Deputy Medical Officer. “We continue to lose more people in BC to the toxic drug crisis than to COVID-19, yet the issue is not receiving the attention it deserves. We need to change the narrative and work together to address existing stigmas surrounding toxic drug use."
To address some of the challenges caused by pandemic restrictions, in 2020 the FNHA swiftly launched the First Nations Virtual Substance Use and Psychiatry Service as part of its commitment to create a range of accessible treatment and healing options for Indigenous people who use substances. The FNHA also supported expanded access to prescription alternatives and Opioid Agonist Therapy. In an effort to keep people safe when they are using drugs, the FNHA developed a comprehensive harm reduction policy, expanded harm reduction education across the province, and transitioned the successful Not-Just-Naloxone training sessions online. The recent launch of a harm reduction campaign uses personal stories to engage and educate on the impacts of the toxic drug crisis on BC First Nations people, their friends, families, and communities.
Public discussion of the toxic drug crisis and its impact on BC First Nations may be difficult and potentially triggering for the many people impacted. The KUU-US Crisis Line is available 24/7 to support Indigenous people in BC.
Toll-Free: 1-800-KUU-US17 (1-800-588-8717)
Adult/Elder: 1-250-723-4050
Child/Youth: 1-250-723-2040
QUOTATIONS
Colleen Erickson, Chair, FNHA
Despite expanded harm reduction education, services and supports for First Nations people, we continue to be disproportionately represented in both COVID-19 and toxic drug events. This reflects the persistence of root causes and the inequity in the provision of health care services and supports for First Nations people in BC.
Dr. Shannon McDonald, Acting Chief Medical Officer, FNHA
The data underscores the immense toll that drug toxicity is having on the lives of Indigenous people and their communities. That the toxic drug crisis continues to wreak havoc on Indigenous people five years after the B.C. government declared a public health emergency is a clear indication there is still much more to be done to resolve this tragic public health issue.
Charlene Belleau, Chair, First Nations Health Council
These new data demonstrate again how the toxic drug crisis disproportionally affects BC First Nations people, and how the concurrent COVID-19 pandemic has been devastating for those struggling with addiction. We know culturally safe harm reduction strategies and adequate funding for treatment are critical steps to reduce the impact of the toxic drug crisis on people and families.
Dr. Bonnie Henry, BC Provincial Health Officer
The COVID-19 pandemic has affected every aspect of our society and has further exacerbated and highlighted the inequities Indigenous communities continue to face in the healthcare system. The year-over-year increase in overdose deaths amongst First Nations men, women and young people is heartbreaking and speaks to the need for a community approach, led by First Nations in collaboration with the provincial system, to unpack the stigma that continues today. I commend the First Nations Health Authority for the steps they have taken, together with Indigenous peoples throughout the province, to encourage people to speak up, to seek support, to reduce stigma and prevent further tragic overdoses in their communities.
Lisa Lapointe, Chief Coroner, BC Coroner's Service
We are experiencing devastating losses across British Columbia as a toxic illicit drug supply takes the lives of our family members, our friends and our co-workers. After decades of criminalizing people experiencing problematic substance use, we now recognize this is a health crisis requiring a compassionate, evidence-based and health-centered response. As the data indicates, the impact of this crisis on Indigenous people is profound, and our response must be culturally safe and available in all parts of our province.
Sheila Malcolmson, Minister of Mental Health and Addictions
This overwhelming loss of life is felt deeply in every community and we mourn with all the families, relatives, friends and caregivers that carry this loss. The collision of the pandemic, the poisoned drug supply and Indigenous-specific racism is at the root of the crisis we see today. Our government continues to work closely with First Nation partners to accelerate actions that will save lives and will address the root causes that are contributing to this tragedy. This work cannot wait and our collective resolve and commitment is more important than ever.
BACKGROUNDER: FNHA ACTIONS TAKEN TO PREVENT OVERDOSE IN 2020-2021
- Distributed more than 18,000 naloxone nasal spray units through community pharmacies, and more than 8,000 units to 90+ First Nations communities. Distributed nearly 8,000 injectable naloxone its to FNHA take-home sites.
- More than 100 people completed Not Just Naloxone training.
- 14 harm reduction champions received community grants of $2,500 each.
- New Harm Reduction Policy includes provision of harm reduction services, expansion of substitution therapies, and support of pharmaceutical alternatives to toxic street drugs.
- Committed to hire 10 Indigenous Harm Reduction Educators and 10 Peer Coordinators to serve First Nations communities in BC.
- Supported 21 rural and remote First Nations communities to improve access to treatment options for opiod use disorder.
- Launched a Virtual Substance use and Psychiatry Service providing access to addictions specialists for assessment, treatment planning, withdrawal management, and pharmaceutical alternatives.
- 223 people received subsidies to access OAT at medical clinics.
- Delivered Indigenous treatment and land-based healing grounded in cultural teachings: 147 initiatives providing mental health, and addictions services.
- Committed to upgrading some existing Treatment and Healing Centres, and to the construction of new healing centres in Vancouver Coastal and Fraser Salish regions.
- Hosted four webinars encouraging more than 450 people to enter into difficult conversations about substance use, encouraging family, friends, and loved ones to share challenges and reframe discussion to include Indigenous strengths and self-determination.
- Created an Indigenous Harm Reduction Community Council, a province-wide network of Indigenous people working on Indigenous approaches to harm reduction, providing knowledge sharing across all regions.
- Supported 188 people to connect to health and housing supports immediately following release from incarceration to address risk of subsequent toxic drug events and death post-release.
- Promoted culturally safe services, strengthening partnerships with Indigenous service providers and health care system partners to address cultural safety and systemic racism in BC health services.
Resources

