(Tansi, pronounced tan seh, is a common Cree greeting. Cree is spoken in several areas of the Northeast.)
Members of the Northern First Nations Health Partnership Committee (NFNHPC) met on Lheidli T’enneh territory November 26, 2019, with representatives from First Nations communities, the First Nations Health Council, the First Nations Health Directors’ Association, the First Nations Health Authority (FNHA) and Northern Health (NH). The committee discussed a range of topics from ambulance services to remote communities, and from funding for land-based healing, to nurse practitioner supports.
Highlights
The meeting began with a prayer, drumming and smudging, setting the tone for a productive day, co-chaired by Penny Anguish and Wilf Adam.
Northern Partnership Accord Evaluation.
Highlights of the updates included the presentation of a preliminary report on the Northern Partnership Accord (NPA) Evaluation. Successes and challenges were noted and there was general agreement to use the report as a guiding document to support changes to the NPA and the Health and Wellness Plan going forward. Once the report has been reviewed, Cathy Ulrich and Nicole Cross will meet to identify next steps.
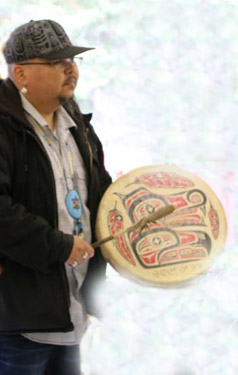
Clayton Gauthier drumming
NFNHPC Working Groups
Mental Wellness Substance Use
The Mental Wellness Substance Use working group has been focused on opioid support services integration. Their report noted that two half-time peer coordinator roles planned for Terrace and Fort St. John are posted and unfilled. A targeted reach-out to potential candidates was suggested as a way to remedy this. The Joint Crisis Response Protocol is another initiative wherein NH supports developing a collaborative framework that outlines areas of consideration and processes to establish and use locally developed protocols between providers and community health staff.
Primary Health Care
The Primary Health Care working group informed the committee that iPads are being used for patients and families in palliative care to provide better specialty services in-home. The FNHA has hired a dietician and food security coordinator to support the holistic work being done in chronic care. Continued work is being done to have electronic medical records integrated across the North; bandwidth, connectivity and financial challenges are slowing the process. A report is being prepared on recruitment and retention, and is nearing completion. A presentation on Primary Care Networks was given, along with the Mobile Primary Care Team update.
Population Public Health
The Population Public Health working group’s report shared that NH is proactively preparing information in case of wildfires and how to best respond afterwards. There is a desire to strengthen cultural humility in the way NH deals with day care licensing in NH and FNHA facilities. Information on the topics of e-cigarettes and cannabis will be shared with all public and independent schools to promote healthy environments.
Cultural Safety
The Cultural Safety working group has set three priorities for the next year: Aboriginal Patient Liaison; patient self-identification; and cultural safety and education. The Indigenous Health team continues to work on improving the role of ceremonial smudging and brushing in the health system, with the goal of removing barriers, myths and issues raised in relation to smoke and fire alarm systems.
Maternal Child Health
The Maternal Child Health discussion centred on the importance of working directly with new mothers and families. The birth alert process within NH has been discontinued. The practice is now to meet with the mother and have a conversation with her to identify what supports she will need to prepare for her baby. Other maternal health initiatives include making universal contraception available in communities; HPV home screening in the Northeast; remote midwifery services; doulas now have a community of practice (a peer-to-peer support network for education and sharing best practices, etc.); and the Aboriginal Head Start on Reserve program has expanded in the North for three additional communities that did not receive provincial funding.
Mobile Support Teams
Since its inception, the Mobile Support Teams (MSTs) network has been a collaborative undertaking, with the involvement of health directors, health services administrators, FNHA and NH on the advisory committees. There are two types of MSTs: the majority (10) are focused on Mental Wellness and Substance Use (MWSU-MST) and one is a Primary Care team. The MWSU-MST members vary based on community needs, but are usually formed around a mental health and addictions nurse, with the addition of a registered social worker and/or mental health and addictions clinicians. The MWSU-MST is built on a collaborative service model informed by the needs and concerns of First Nations communities. Its aim is to improve culturally responsive care and services for communities and individuals, and integrate into larger health systems support. The network of MSTs, funded by the Joint Project Board, has grown from three teams to the current eleven, situated in all three sub-regions. While recruitment and retention concerns continue, the model is successful.
Aboriginal Patient Liaison Workers
Aboriginal Patient Liaison Workers (APLW) roles are key to cultural safety in health services for First Nations in the region. The APLW program has been evaluated, resulting in twenty-three recommendations around knowledge sharing and promotion; support for APLWs; program delivery; and longer term strategic planning. Currently, eleven of fourteen positions are filled across the North, with two new FTEs being added. The APLWs are key to enhancing communications in general, and are well positioned to promote the MSTs and to encourage health directors in their areas to do so, too. The value of each APLW is recognized by the committee, and all members are committed to continued support of this work.
Men’s Wellness Programs
Men’s wellness programs in the North have grown exponentially. Starting with six pilot sites in 2017, there are now more than twenty-two. The investment has been modest, but the rewards are significant and truly making a difference at the community level. Men gather with a facilitator, elder and peers to support each other, discuss health issues, relationships, roles in the community. They regularly organize fundraisers and activities or provide services to elders and others that are much appreciated.
And Finally . . .
There were several new members from the Northern Regional Table who noted the good work being done by the NFNHPC. One member summarized it with the following: “Amazing partnership that we should capitalize and continue to build on.” The work shows how commitment, respect, perseverance and dedication are evident when all parties have a common goal. We wish to acknowledge the efforts of all members of the committee and thank them.

