Working together to prevent suicide, promote hope and resiliency

A Message from Dr. Nel Wieman, Senior Medical Officer, Mental Health & Wellness
Today, September 10, is World Suicide Prevention Day, a time to talk openly about this very important – indeed, life-or-death – topic. "Working Together to Prevent Suicide," The International Association for Suicide Prevention's theme for 2018, works well for First Nations communities in BC and aligns with the First Nations Health Authority's Perspective on Health and Wellness. As does the Canadian Association for Suicide Prevention's recommended strategy of promoting hope and resiliency as central to preventing suicide.
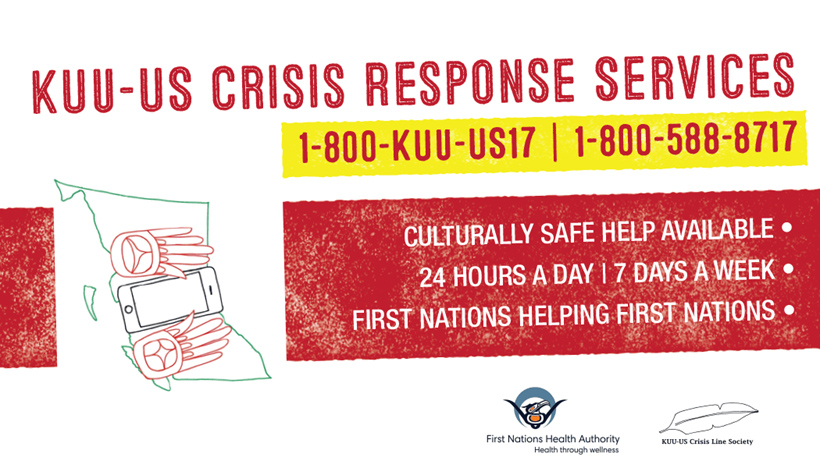
In fact, building upon the intergenerational resilience and strength Indigenous people have shown despite all that has been done over the years and is still being done today, Indigenous organizations, including the FNHA, have been working together with our partners to change the focus around suicide to one that is more life- and hope-affirming. For example, the FNHA created the "Hope, Help & Healing Suicide Prevention, Intervention, and Postvention Toolkit," which is available to all First Nations communities in BC. We also partnered with KUU-US Crisis Line Society, an Indigenous-run organization that works to reduce the stigma and shame associated with mental health or life crisis issues that might lead to thoughts of suicide, and also provides a culturally safe 24/7 crisis hotline (see poster below).
Another example of changing the focus is Nunavut's "Embrace Life Council," which has worked on various suicide prevention initiatives in that territory since 2004. The language is changing to one of hope and connection.
Public health campaigns such as the Bell-sponsored "Let's Talk" have also contributed to a more open dialogue around mental health and wellness, and reduced the stigma and shame of having a mental illness. But one does not necessarily have to have a mental illness to feel suicidal or to make a suicide attempt. Sometimes, these types of campaigns put more focus on encouraging someone in distress to reach out – not in itself a bad thing – but what if one is distressed and cannot or will not reach out? How do we, as family and community members, be helpful to a person who may be considering suicide?
In my experience as a psychiatrist, I've found that people become suicidal when they are emotionally distressed and feel they've run out of options, have no way out of an unwanted situation, no possibility of relief. Part of how we can be helpful to such a person is to have them see that they do in fact have other options available to them, and that feelings are not always persistent. They can continue to talk to a supportive friend, family member, relative, community member or health professional. But how do we know when someone we care about is feeling suicidal and not (yet) talking about it?
There are a number of symptoms and signs that are generally thought to be indicative that someone may be feeling suicidal:
• Talking about wanting to die or kill oneself
• Looking for a way to kill oneself; having access to a way (e.g., weapon)
• Talking about feeling hopeless or having no purpose
• Talking about feeling trapped or in unbearable pain
• Talking about being a burden
• Using alcohol or drugs more frequently
• Being anxious, agitated or restless; having extreme mood swings
• Experiencing sleep issues (e.g., increased / decreased)
• Withdrawing; being/feeling socially isolated
• Exhibiting rage or talking about revenge
• Searching for ways to kill oneself: online or physically
• Talking/writing/posting on social media about death and suicide
But the easiest answer to the question of "how do we know if someone is suicidal" can be simple: reach out and ask them how they're really feeling. Instead of putting the onus on the person in distress to reach out, let's consider regularly checking in with those we care about, to see where they are at. And of course, if someone discloses to us that they are feeling distressed and possibly suicidal, instead of minimizing what they may be feeling, let's be supportive and active in our response – let's help them access the mental health support they need. It is in this way that we can work together to prevent suicide. If we continue to be proactive about our own and our loved ones' mental wellness, we may be able to avert a crisis from developing. This is one way of promoting hope and resiliency. And when we say "Let's talk," we can also mean "I'm reaching out to you, I'm willing to listen to what you have to say, I'm here for you and I'll help you if you need it." Let's consider starting the conversation.
This World Suicide Prevention Day, let's remember to reach out and stay connected. For more information about suicide prevention, see https://suicideprevention.ca/More-on-suicide-prevention. To find out about accessing mental health supports through FNHA Health Benefits, visit http://www.fnha.ca/benefits/mental-health or contact this FNHA department at healthbenefits@fnha.ca.

